×
Il semble que vous utilisiez une version obsolète de internet explorer. Internet explorer n'est plus supporté par Microsoft depuis fin 2015. Nous vous invitons à utiliser un navigateur plus récent tel que Firefox, Google Chrome ou Microsoft Edge.

Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Vous devez être membre pour accéder aux vidéos Incathlab sans limitation. Inscrivez vous gratuitement en moins d'une minute et accédez à tous les services Incathlab ! Vous avez aussi la possibilité de vous connecter directement avec votre compte facebook ou twitter en cliquant sur login en haut à droite du site.
Inscription Connexion
Inscription Connexion
This didactic procedure regards a 60 years old man presenting a severe left lower limb claudication with rest pain (stage 3). The patient has a history of two femoro-infrapopliteal venous bypasses which both occluded shortly after. Multimodality imaging revealed a long occlusion of the femoropopliteal axis with a severely diseased posterior tibial artery. A previous antegrade attempt of recanalization failed due to severe calcification. No retrograde attempt was done due to severe claudication. The patient has finally undergone a percutaneous femoropopliteal bypass.
Educational objectives
- Define the indication of percutaneous femoro-popliteal bypass (PFPB) in severe lower limb disease.
- Plan a step-by-step procedure of PFBP.
- How to manage antegrade and retrograde access?
- How to choose the accurate spots for the implantation of PFPB: proximal and distal implantation.
- Selecting the appropriate devices : guidewires, microcatheters, guiding catheter, balloons and covered stents
- How to modify a guiding catheter for a coaxial transseptal needle system?
- How to safely perform a puncture using transseptal needle through occluded femoral artery.
- How to safely perform an externalization and extra-vessel trajectory?
- Tips and tricks to a successful puncture and reentry.
- What are adjunctive pharmacotherapies?
Step-by-step procedure: supra-articular femoropopliteal percutaneous bypass
1) Access sites:
- Antegrade femoral access: 6 French sheath and 8 French sheath for final stenting.
- Retrograde access through the anterior tibial artery (ATA).
2) Retrograde recanalization:
- V-18™ wire and Terumo 0.035” angled stiff Glidewire® with the support of TrailBlazer™ microcatheter.
- Advancement of knuckled wire through tibioperoneal trunk (TPT) subintimally until the landing zone (distal third of left superficial femoral artery (FSA))
- Pre-dilatation: OTW Armada balloons : 3*60 mm then 5*60 mm.
3) Preparation of the landing zone:
- Predilatation: OTW Armada balloon 5*60 mm.
- Use the balloon in place to identify the landing zone..
4) Preparation of the transseptal needle:
- 6 French guiding catheter cut to obtain a shorter one at the level of the transseptal needle curve
- Insertion of the transseptal needle in the modified 6 French guiding catheter to protect the needle (avoid vessel perforation or dissection).
- Coaxial system: direct the transseptal needle and puncture safely.
5) Externalisation and extravessel trajectory :
- Puncture of the vessel wall toward the medial side of the proximal cap of the occluded vessel (avoid collateral vessels).
- Injection of diluted Lidocaïne (0.1%) locally.
- Advancement of the knuckled Terumo 0.035’’ angled Glidewire® into the extravascular space, paralleled to the native vessel (following calcifications) with the support of the guiding catheter.
6) Reentry
- Balloon dilatation from retrograde access at the reentry site (REVERSE CART technique).
- Puncture at the reentry site: balloon and guidewire from retrograde access serve as a benchmark, and orthogonal views.
- Pre-dilatation of the reentry site: Armada OTW balloon 4*60 mm
- Positioning of the guiding catheter downstream to the reentry site, inside the vessel structure.
7) Stenting:
- Exchange to a support guidewire: Lunderquist Extra Stiff 0.035’’ guidewire.
- Exchange to an 8 French sheath 45cm which is advanced downstream to the distal reentry point.
- Stenting the reentry point: Covera™ stent 6*100 mm.
- Stenting the extra-vessel trajectory: Viabahn®7*150 mm with long overlapping.
- Stenting the exit point Viabahn® 7*80 mm with long overlapping.
8) Antegrade angioplasty:
- Predilatation and stenting of the popliteal artery.
- Remove ATA sheath and balloon hemostasis.
9) Post dilatation of the covered stents
10) Medical adjunctive treatments
- Pre-procedural: Heparin and Antibioprophylaxis.
- Post procedural: Triple therapy: Aspirin 75mg o.d. + Clopidogrel 75mg o.d. + Enoxaparin 100 UI/kg b.i.d. : 15 days.
- DUS 15 days after.
- Stop Clopidogrel and continue Aspirin 75mg b.i.d and NAOC.
Bibliography
Procedure
- Procedure time: 105 min
- Exposure time: 44 min
- Exposure: 190 mGy
- Contrast volume: 100 ml Visipaque 320
Date du tournage : 08/11/2019
Dernière mise à jour : 11/05/2021
Dernière mise à jour : 11/05/2021
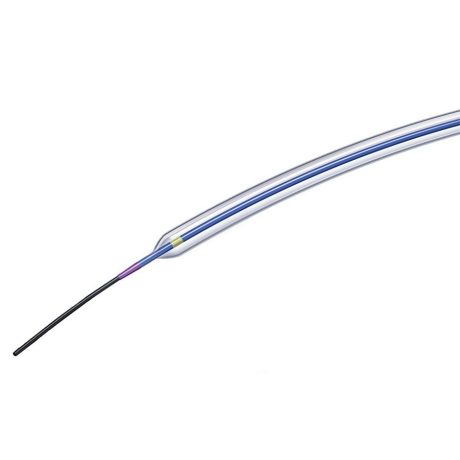
Sterling™ PTA Balloon dilatation catheter / Boston Scientific
PTA Balloon dilatation catheter
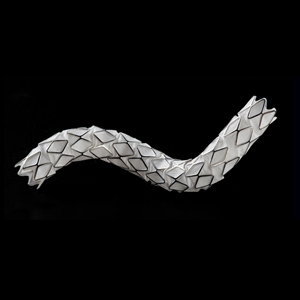
GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis / Gore
Flexible strength. Proven success.
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Partager
Suggestions
Mardi 27 avril 2021 de 15h à 16h (GMT+2)
Honolulu : Mardi 27 avril 2021 de 04h à 05h (GMT+2)
San Francisco : Mardi 27 avril 2021 de 07h à 08h (GMT+2)
New York : Mardi 27 avril 2021 de 10h à 11h (GMT+2)
Buenos Aires : Mardi 27 avril 2021 de 11h à 12h (GMT+2)
Reykjavik : Mardi 27 avril 2021 de 14h à 15h (GMT+2)
London / Dublin : Mardi 27 avril 2021 de 15h à 16h (GMT+2)
Paris / Berlin : Mardi 27 avril 2021 de 16h à 17h (GMT+2)
Istanbul : Mardi 27 avril 2021 de 17h à 18h (GMT+2)
Moscou / Dubaï : Mardi 27 avril 2021 de 18h à 19h (GMT+2)
Bangkok : Mardi 27 avril 2021 de 21h à 22h (GMT+2)
Shanghai : Mardi 27 avril 2021 de 22h à 23h (GMT+2)
Tokyo : Mardi 27 avril 2021 de 23h à 00h (GMT+2)
Sydney : Mercredi 28 avril 2021 de 01h à 02h (GMT+2)
Wellington : Mercredi 28 avril 2021 de 03h à 04h (GMT+2)
San Francisco : Mardi 27 avril 2021 de 07h à 08h (GMT+2)
New York : Mardi 27 avril 2021 de 10h à 11h (GMT+2)
Buenos Aires : Mardi 27 avril 2021 de 11h à 12h (GMT+2)
Reykjavik : Mardi 27 avril 2021 de 14h à 15h (GMT+2)
London / Dublin : Mardi 27 avril 2021 de 15h à 16h (GMT+2)
Paris / Berlin : Mardi 27 avril 2021 de 16h à 17h (GMT+2)
Istanbul : Mardi 27 avril 2021 de 17h à 18h (GMT+2)
Moscou / Dubaï : Mardi 27 avril 2021 de 18h à 19h (GMT+2)
Bangkok : Mardi 27 avril 2021 de 21h à 22h (GMT+2)
Shanghai : Mardi 27 avril 2021 de 22h à 23h (GMT+2)
Tokyo : Mardi 27 avril 2021 de 23h à 00h (GMT+2)
Sydney : Mercredi 28 avril 2021 de 01h à 02h (GMT+2)
Wellington : Mercredi 28 avril 2021 de 03h à 04h (GMT+2)
Preserving Coronary Access After TAVI
Case of the month: September 2021
Partager
Long Femoral Occlusion (35 cm) - Subintimal crossing and extra long stenting
Case of the month: July 2017
Partager
Complex Valve-in-Valve (VIV) TAVI for Aortic bioprosthesis dysfunction
Case of the month: July 2018
Partager
Calcified distal Left Main and LAD stenoses - Rotablation treatment and IVUS evalutation
Case of the month: June 2017
Partager