×
It looks like you're using an obsolete version of internet explorer. Internet explorer is no longer supported by Microsoft since the end of 2015. We invite you to use a newer browser such as Firefox, Google Chrome or Microsoft Edge.

Become an Incathlab member and receive full access to its content!
You must be an Incathlab member to access videos without any restrictions. Register for free in one minute and access all services provided by Incathlab.You will also be able to log into Incathlab from your Facebook or twitter account by clicking on login on the top-right corner of Incathlab website.
Registration Login
Registration Login
This didactic procedure concerns a left side ilio-femoral chronic venous obstruction.
Educationnel objectives
- Plan a step-by-step ilio-femoral chronic venous obstruction procedure.
- Materials choice: guidewires, support catheters, balloons and dedicated stents.
- Learn different techniques to advance and manipulate guidewire through the occlusion.
- How to proceed to an optimal lesion preparation?
- Tips and tricks for a good positioning and implantation of the stents.
- Advantage and usefulness of IVUS to optimize the procedure?
- Importance of adjunctive pharmacotherapies?
Step-by-step procedure: Left internal carotid artery stenting
1) Access sites:
- Femoral access: Echo guided puncture at mid femoral vein (Sheath position: upstream to the lesion and avoid conflict between the sheath and the occlusion).
- 7 French sheath.
- First contrast injection to establish vein cartography with different collaterals.
- Anticoagulation.
2) Recanalization
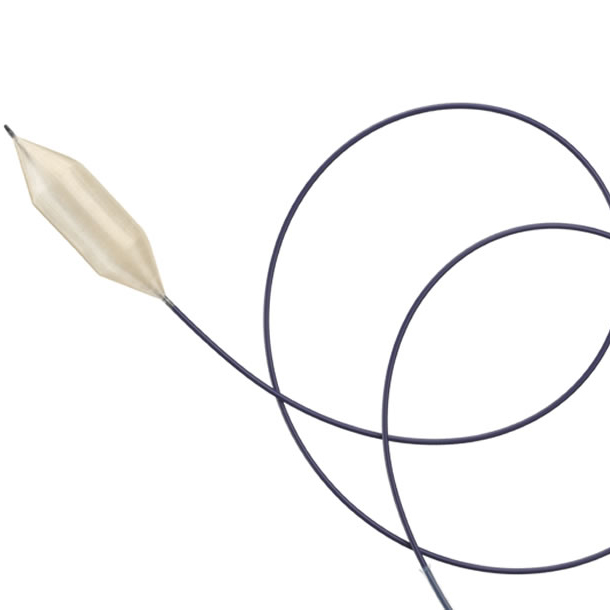
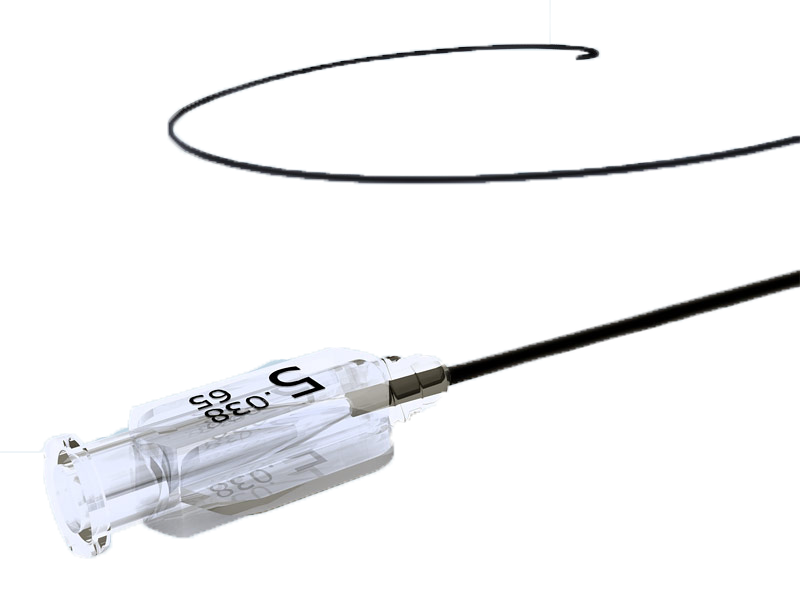
- Park an angled stiff Terumo® RADIOFOCUS® wire 0.035” at the entry of the occlusion.
- Advance the wire through the occlusion: with a combination of torque and push movements with the support of a vertebral Glidecath® TERUMO®catheter 4Fr.
- Improve wire support after advancing through the lesion with a support catheter TrailBlazer™ catheter (after 2-3cm through the occlusion, improving the support to ensure enough pushability is extremely important).
- Check the trajectory of the wire in different orthogonal projections to be sure that the wire is in the vessel structure.
- Advancement with the loop wire technique in the common iliac vein (in case of failure to advance with the straight tip of the wire).
- Angio control to check the progression of the wire.
- Tips and tricks: To be sure that you are in the IVC: In the lateral projection, the wire or the catheter should be ventral to the vertebral body.
- After crossing the lesion exchange with a 0.035” Amplatz super stiff™ wire.
- Balloon pre-dilatation: Balloon pre-dilatation should be done from healthy -to- healthy part of the vein. A 7*60 mm Mustang® balloon used to dilate at the distal part of the occlusion (usually start at the proximal part of the occlusion unless facing difficulties to progress the balloon through the occlusion).
- Pre-dilatation with a 12*80mm Mustang® balloon.
- Stent diameter choice: external iliac vein: 12-14cm and common iliac vein: 14 -16 cm.
- IVUS control VISION PV 8.5 Fr 0.035”*90cm : Useful information from IVUS: results of the pre-dilatation, maximum point of the compression, length and diameter of the stent and landing zone of the stent (in addition to reducing contrast injection and radiation).
- Positioning the stent from healthy to health part of the vein.
- Use a dedicated vein stent ATLAS GOLD® 14*60mm, ABRE™ STENT 14*150mm, ABRE™ stent 12-80mm (avoid overlapping at the level of the ligament area).
- Post dilation of the stent.
- IVUS control : stent opening geometry and control the landing zone.
- Final angio control: stent patency with no visualization of the deep femoral vein and the collaterals.
- Adjunctive therapies: Aggressive anticoagulation to maintain stent patency.
- Femoral access: Echo guided puncture at mid femoral vein (Sheath position: upstream to the lesion and avoid conflict between the sheath and the occlusion).
- 7 French sheath.
- First contrast injection to establish vein cartography with different collaterals.
- Anticoagulation.
Protocol
- Procedure time 125 min
- Exposure time 29.91 min
- Exposure 11463 mGy.cm²
- Contrast vomule :70ml Ioméron 350
Bibliography
-
Taha MAH, Busuttil A, Bootun R, Thabet BAH, Badawy AEH, Hassan HA, et al. A clinical guide to Deep venous stenting for chronic iliofemoral venous obstruction. J Vasc Surg Venous Lymphat Disord. mai 2021;S2213333X21002195.
-
Raju S. Best management options for chronic iliac vein stenosis and occlusion. J Vasc Surg. avr 2013;57(4):1163‑9.
-
Kölbel T, Lindh M, Åkesson M, Wassèlius J, Gottsäter A, Ivancev K. Chronic Iliac Vein Occlusion: Midterm Results of Endovascular Recanalization. J Endovasc Ther. août 2009;16(4):483‑91.
-
Rollo JC, Farley SM, Jimenez JC, Woo K, Lawrence PF, DeRubertis BG. Contemporary outcomes of elective iliocaval and infrainguinal venous intervention for post-thrombotic chronic venous occlusive disease. J Vasc Surg Venous Lymphat Disord. nov 2017;5(6):789‑99.
-
Seager MJ, Busuttil A, Dharmarajah B, Davies AH. Editor’s Choice – A Systematic Review of Endovenous Stenting in Chronic Venous Disease Secondary to Iliac Vein Obstruction. Eur J Vasc Endovasc Surg. janv 2016;51(1):100‑20.
-
Wittens C, Davies AH, Bækgaard N, Broholm R, Cavezzi A, Chastanet S, et al. Editor’s Choice – Management of Chronic Venous Disease. Eur J Vasc Endovasc Surg. juin 2015;49(6):678‑737.
-
Hood DB, Alexander JQ. Endovascular management of iliofemoral venous occlusive disease. Surg Clin North Am. oct 2004;84(5):1381‑96
-
Menez C, Rodiere M, Ghelfi J, Seinturier C, Martinelli T, Imbert B, et al. Endovascular Treatment of Post-thrombotic Venous Ilio-Femoral Occlusions: Prognostic Value of Venous Lesions Caudal to the Common Femoral Vein. Cardiovasc Intervent Radiol. août 2019;42(8):1117‑27.
-
Friedrich de Wolf MA, Arnoldussen CW, Grommes J, Hsien SG, Nelemans PJ, de Haan MW, et al. Minimally invasive treatment of chronic iliofemoral venous occlusive disease. J Vasc Surg Venous Lymphat Disord. avr 2013;1(2):146‑53.
-
Lichtenberg M, de Graaf R, Erbel C. Standards for recanalisation of chronic venous outflow obstructions. Vasa. 1 juin 2018;47(4):259‑66
-
Lichtenberg M, Stahlhoff S, Özkapi A, de Graaf R. Braided nitinol stent for chronic iliofemoral venous disease – the real-world BLUEFLOW registry. Vasa. sept 2021;50(5):372‑7.
-
Hans SS, Conrad MF, éditeurs. Vascular and endovascular complications: a practical approach. First edition. Boca Raton, FL: CRC Press; 2021.
-
Schleimer K, Barbati ME, Grommes J, Hoeft K, Toonder IM, Wittens CHA, et al. Update on diagnosis and treatment strategies in patients with post-thrombotic syndrome due to chronic venous obstruction and role of endovenous recanalization. J Vasc Surg Venous Lymphat Disord. juill 2019;7(4):592‑600.
-
Soosainathan A, Moore HM, Gohel MS, Davies AH. Scoring systems for the post-thrombotic syndrome. J Vasc Surg. janv 2013;57(1):254‑61.
-
Raju S, Neglén P. Percutaneous recanalization of total occlusions of the iliac vein. J Vasc Surg. août 2009;50(2):360‑8.
-
Majdalany B, Khaja M, Williams D. Intravascular Ultrasound-Guided Intervention for May–Thurner Syndrome. Semin Interv Radiol. juin 2017;34(02):201‑7.
-
Li Y, Zou Y, Wang S, Li J, Jing X, Yang M, et al. A Pilot Study of the FRAIL Scale on Predicting Outcomes in Chinese Elderly People With Type 2 Diabetes. J Am Med Dir Assoc. 2015;16(8):714.e7-714.e12.
-
Lichaa H, Lakhter V, Mohan J, Kerrigan J, Secemesky E. Intravascular Ultrasound Use for Iliac Vein Interventions. Curr Cardiovasc Imaging Rep. août 2021;14(8):8.
-
Marteslo JP, Makary MS, Khabiri H, Flanders V, Dowell JD. Intravascular Ultrasound for the Peripheral Vasculature—Current Applications and New Horizons. Ultrasound Med Biol. févr 2020;46(2):216‑24.
Shooting date : 2020-09-07
Last update : 2021-11-05
Last update : 2021-11-05
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Share
Join the Discussion
Suggestions
Wednesday, October 10th 2018 from 12pm to 01:30pm (GMT+2)
Honolulu : Wednesday, October 10th 2018 from 01am to 02:30am (GMT+2)
San Francisco : Wednesday, October 10th 2018 from 04am to 05:30am (GMT+2)
New York : Wednesday, October 10th 2018 from 07am to 08:30am (GMT+2)
Buenos Aires : Wednesday, October 10th 2018 from 08am to 09:30am (GMT+2)
Reykjavik : Wednesday, October 10th 2018 from 11am to 12:30pm (GMT+2)
London / Dublin : Wednesday, October 10th 2018 from 12pm to 01:30pm (GMT+2)
Paris / Berlin : Wednesday, October 10th 2018 from 01pm to 02:30pm (GMT+2)
Istanbul : Wednesday, October 10th 2018 from 02pm to 03:30pm (GMT+2)
Moscou / Dubaï : Wednesday, October 10th 2018 from 03pm to 04:30pm (GMT+2)
Bangkok : Wednesday, October 10th 2018 from 06pm to 07:30pm (GMT+2)
Shanghai : Wednesday, October 10th 2018 from 07pm to 08:30pm (GMT+2)
Tokyo : Wednesday, October 10th 2018 from 08pm to 09:30pm (GMT+2)
Sydney : Wednesday, October 10th 2018 from 10pm to 11:30pm (GMT+2)
Wellington : Thursday, October 11th 2018 from 12am to 01:30am (GMT+2)
San Francisco : Wednesday, October 10th 2018 from 04am to 05:30am (GMT+2)
New York : Wednesday, October 10th 2018 from 07am to 08:30am (GMT+2)
Buenos Aires : Wednesday, October 10th 2018 from 08am to 09:30am (GMT+2)
Reykjavik : Wednesday, October 10th 2018 from 11am to 12:30pm (GMT+2)
London / Dublin : Wednesday, October 10th 2018 from 12pm to 01:30pm (GMT+2)
Paris / Berlin : Wednesday, October 10th 2018 from 01pm to 02:30pm (GMT+2)
Istanbul : Wednesday, October 10th 2018 from 02pm to 03:30pm (GMT+2)
Moscou / Dubaï : Wednesday, October 10th 2018 from 03pm to 04:30pm (GMT+2)
Bangkok : Wednesday, October 10th 2018 from 06pm to 07:30pm (GMT+2)
Shanghai : Wednesday, October 10th 2018 from 07pm to 08:30pm (GMT+2)
Tokyo : Wednesday, October 10th 2018 from 08pm to 09:30pm (GMT+2)
Sydney : Wednesday, October 10th 2018 from 10pm to 11:30pm (GMT+2)
Wellington : Thursday, October 11th 2018 from 12am to 01:30am (GMT+2)
Calcium, Dissections, No Stent Zones: How leading centers are fighting the last challenges in the SF...
Live from University Hospital Leipzig
Share
Wednesday, February 12th 2020 | 12pm to 01:30pm (EST) - 06pm to 07:30pm (GMT+1)
Honolulu : Wednesday, February 12th 2020 from 07am to 08:30am (GMT+1)
San Francisco : Wednesday, February 12th 2020 from 09am to 10:30am (GMT+1)
New York : Wednesday, February 12th 2020 from 12pm to 01:30pm (GMT+1)
Buenos Aires : Wednesday, February 12th 2020 from 02pm to 03:30pm (GMT+1)
London / Dublin : Wednesday, February 12th 2020 from 05pm to 06:30pm (GMT+1)
Paris / Berlin : Wednesday, February 12th 2020 from 06pm to 07:30pm (GMT+1)
Istanbul : Wednesday, February 12th 2020 from 07pm to 08:30pm (GMT+1)
Moscou / Dubaï : Wednesday, February 12th 2020 from 09pm to 10:30pm (GMT+1)
Bangkok : Thursday, February 13th 2020 from 12am to 01:30am (GMT+1)
Shanghai : Thursday, February 13th 2020 from 01am to 02:30am (GMT+1)
Tokyo : Thursday, February 13th 2020 from 02am to 03:30am (GMT+1)
Sydney : Thursday, February 13th 2020 from 03am to 04:30am (GMT+1)
Wellington : Thursday, February 13th 2020 from 05am to 06:30am (GMT+1)
San Francisco : Wednesday, February 12th 2020 from 09am to 10:30am (GMT+1)
New York : Wednesday, February 12th 2020 from 12pm to 01:30pm (GMT+1)
Buenos Aires : Wednesday, February 12th 2020 from 02pm to 03:30pm (GMT+1)
London / Dublin : Wednesday, February 12th 2020 from 05pm to 06:30pm (GMT+1)
Paris / Berlin : Wednesday, February 12th 2020 from 06pm to 07:30pm (GMT+1)
Istanbul : Wednesday, February 12th 2020 from 07pm to 08:30pm (GMT+1)
Moscou / Dubaï : Wednesday, February 12th 2020 from 09pm to 10:30pm (GMT+1)
Bangkok : Thursday, February 13th 2020 from 12am to 01:30am (GMT+1)
Shanghai : Thursday, February 13th 2020 from 01am to 02:30am (GMT+1)
Tokyo : Thursday, February 13th 2020 from 02am to 03:30am (GMT+1)
Sydney : Thursday, February 13th 2020 from 03am to 04:30am (GMT+1)
Wellington : Thursday, February 13th 2020 from 05am to 06:30am (GMT+1)
An Effective Approach for Challenging Cases: Versatility of Directional Atherectomy & Clinical Appli...
SOLVING UNMET NEEDS in Peripheral Vascular: episode 2
Share
May 2012
Honolulu : Thursday, May 24th 2012 from 05:59am to 08:13am (GMT+2)
San Francisco : Thursday, May 24th 2012 from 08:59am to 11:13am (GMT+2)
New York : Thursday, May 24th 2012 from 11:59am to 02:13pm (GMT+2)
Buenos Aires : Thursday, May 24th 2012 from 12:59pm to 03:13pm (GMT+2)
Reykjavik : Thursday, May 24th 2012 from 03:59pm to 06:13pm (GMT+2)
London / Dublin : Thursday, May 24th 2012 from 04:59pm to 07:13pm (GMT+2)
Paris / Berlin : Thursday, May 24th 2012 from 05:59pm to 08:13pm (GMT+2)
Istanbul : Thursday, May 24th 2012 from 06:59pm to 09:13pm (GMT+2)
Moscou / Dubaï : Thursday, May 24th 2012 from 07:59pm to 10:13pm (GMT+2)
Bangkok : Thursday, May 24th 2012 from 10:59pm to 01:13am (GMT+2)
Shanghai : Thursday, May 24th 2012 from 11:59pm to 02:13am (GMT+2)
Tokyo : Friday, May 25th 2012 from 12:59am to 03:13am (GMT+2)
Sydney : Friday, May 25th 2012 from 02:59am to 05:13am (GMT+2)
Wellington : Friday, May 25th 2012 from 04:59am to 07:13am (GMT+2)
San Francisco : Thursday, May 24th 2012 from 08:59am to 11:13am (GMT+2)
New York : Thursday, May 24th 2012 from 11:59am to 02:13pm (GMT+2)
Buenos Aires : Thursday, May 24th 2012 from 12:59pm to 03:13pm (GMT+2)
Reykjavik : Thursday, May 24th 2012 from 03:59pm to 06:13pm (GMT+2)
London / Dublin : Thursday, May 24th 2012 from 04:59pm to 07:13pm (GMT+2)
Paris / Berlin : Thursday, May 24th 2012 from 05:59pm to 08:13pm (GMT+2)
Istanbul : Thursday, May 24th 2012 from 06:59pm to 09:13pm (GMT+2)
Moscou / Dubaï : Thursday, May 24th 2012 from 07:59pm to 10:13pm (GMT+2)
Bangkok : Thursday, May 24th 2012 from 10:59pm to 01:13am (GMT+2)
Shanghai : Thursday, May 24th 2012 from 11:59pm to 02:13am (GMT+2)
Tokyo : Friday, May 25th 2012 from 12:59am to 03:13am (GMT+2)
Sydney : Friday, May 25th 2012 from 02:59am to 05:13am (GMT+2)
Wellington : Friday, May 25th 2012 from 04:59am to 07:13am (GMT+2)
Discover the difference drug elution makes in the SFA with Zilver PTX stents:
Max Amor, Flavio Airoldi ,Peter Gaines, William Kai,Jorg Tessarek
Share













Mangesh T. Highly impressed with Proper guidance, Good Selection of Hardware materials, devices used & IR Techniques applied for the Re-Vascularisation of Chronically Occluded (Thrombotic) Left ilio-femoral Venous tract. Cause offcourse May-Thurner’s Compression. Few Questions to Main operator Dr. Houman Jalaie Sir are as follows-
1) Why Atlas gold high pressure balloon used in Post Stenting Dilatation when more pressure is needed in Pre-dilatation and breaking of Chronic fibrotic synaechie in Venous lumen?
2) Mustang has 24 atm bursting pressure while Atlas Gold & Conquest PTA Ballons has 30-40 atm bursting pressure.
3) How Vessel preparation prior to Dedicated Venous Stenting matters more?
4) Can we use Popliteal Vein Access site instead of Mid thigh SFV Site? so that 10 Fr Introducer sheath can be easily fixed and Large bore Stent deployment possible with long working shaft.
5) How aggressively , How long Post Venous Stenting Anticoagulation Therapy followed? What about Surviellence & follow up check ups Schedule in this case?