×
Il semble que vous utilisiez une version obsolète de internet explorer. Internet explorer n'est plus supporté par Microsoft depuis fin 2015. Nous vous invitons à utiliser un navigateur plus récent tel que Firefox, Google Chrome ou Microsoft Edge.
My Player placeholder

Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Vous devez être membre pour accéder aux vidéos Incathlab sans limitation. Inscrivez vous gratuitement en moins d'une minute et accédez à tous les services Incathlab ! Vous avez aussi la possibilité de vous connecter directement avec votre compte facebook ou twitter en cliquant sur login en haut à droite du site.
Inscription Connexion
Inscription Connexion
19029 vues
This didactic procedure concerns a 62 years old man, presenting severe right limb intermittent claudication (Rutherford 3) & long proximal SFA lesion with subsequent short occlusion.
It was treated by contralateral and retrograde approach, the lesion was prepared with directional atherectomy & a new cutting balloon (Chocolate-Medtronic). A good final result was obtained with DCB angioplasty.
Educational objectives
- How to deal with extensive SFA disease.
- How to performSFA retrograde puncture, crossing and guidewire externalization.
- Effectivness of Directional atherectomy in long SFA lesions.
- Optimal vessel preparation with combined atherectomy & cutting balloon.
- How to leave Nothing behind.
Step-by-Step description
- Left femoral access 7F (Contralateral approach).
- Crossover approach with 6F long sheath assisted by Admiral 6x40mm balloon.
- Approach lesion with 0.018" Command guidewire supported by Trailblazer microcatheter.
- After Command & Connect guidewires failure, a retrograde approach is decided.
- Retrograde puncture of the distal right SFA.
- Retrograde crossing of the lesion & externalization of the command over a BER catheter.
- Filter placment in the distal popliteal artery.
- predilatation with 3.5mm balloon of the occluded zone.
- Directional atherectomy using a HawkOne device 7F.
- Balloon dilatation with a 5x80mm balloon : distal & proximal SFA.
- Second directional atherectomy run.
- Distal SFA dilatation with Chocolate 6x40mm balloon (Medtronic).
- Multilevel dilatation with DCB : IN PACT Pacific 5x120mm (Medtronic)
- Distal filter retreiving Spider 7mm (Medtronic).
- Final angiographic control.
Protocol
- Procedure time: 90 min
- Exposure time: 29 min
- Exposure: 321 mGy
-
Contrast volume: 120 ml
Biobliography
-
-
Combined HawkOne directional atherectomy and paclitaxel-coated balloon angioplasty for isolated calcified popliteal artery lesion: a no-stent approach to lower extremity endovascular revascularization. - Article
Authors: Loffroy R, Chevallier O, Falvo N, Gehin S, Midulla M, Galland C.
Publication:doi: 10.21037/qims.2018.03.10.
-
Directional Atherectomy Followed by a Paclitaxel-Coated Balloon to Inhibit Restenosis and Maintain Vessel Patency: Twelve-Month Results of the DEFINITIVE AR Study. - Article
Authors: Zeller T, Langhoff R, Rocha-Singh KJ
Publication doi:10.1161/CIRCINTERVENTIONS.116.004848.
-
Debulking Atherectomy in the Peripheral Arteries: Is There a Role and What is the Evidence? - Artice
Authors: Katsanos K, Spiliopoulos S, Reppas L, Karnabatidis D.
Publication doi: 10.1007/s00270-017-1649-6. Epub 2017 Apr 27.
-
Combined treatment of heavy calcified femoro-popliteal lesions using directional atherectomy and a paclitaxel coated balloon: One-year single centre clinical results. - Article
Authors: Cioppa A, Stabile E, Popusoi G, Salemme L, Cota L
Publication doi: 10.1016/j.carrev.2012.04.007. Epub 2012 May 25.
-
A prospective, multi-center study of the chocolate balloon in femoropopliteal peripheral artery disease: The Chocolate BAR registry. - Article
Authors: Mustapha JA, Lansky A, Shishehbor M, Miles McClure J, Johnson S, Davis T, Makam P, Crowder W, Konstantino E, Attaran RR; Chocolate Bar Investigators.
Publication doi: 10.1002/ccd.27565. Epub 2018 Mar 7.
Date du tournage : 09/10/2018
Dernière mise à jour : 11/05/2021
Dernière mise à jour : 11/05/2021
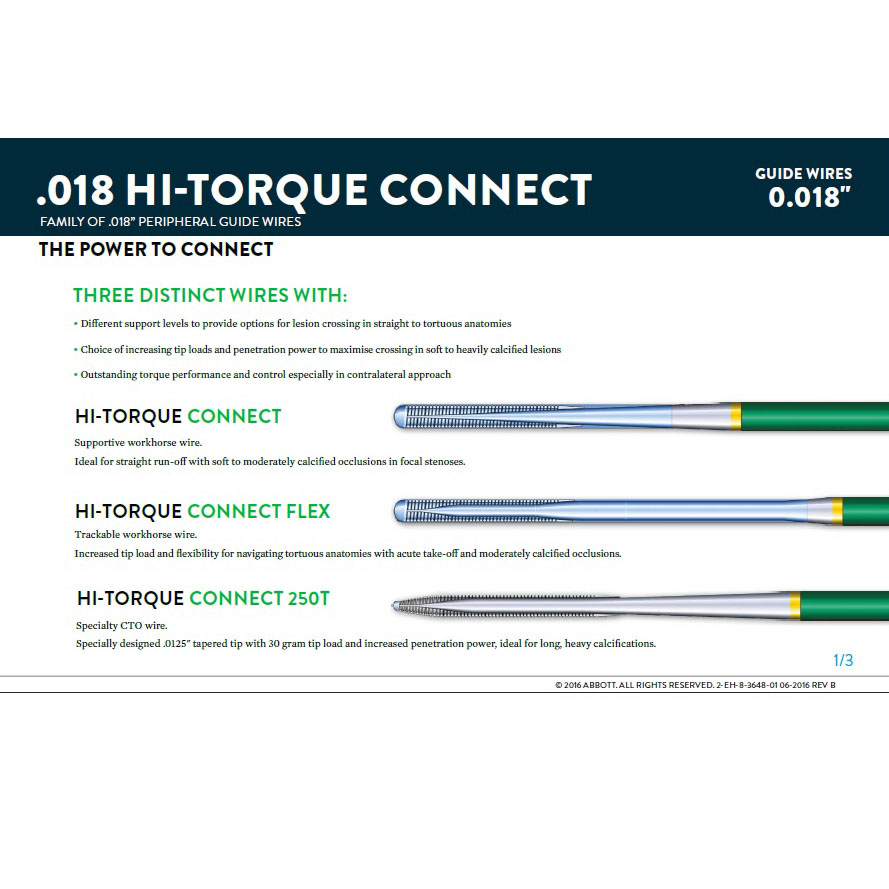
Hi-Torque Connect 0.018" Guide Wire Family / Abbott
A family of 0.018” wires designed for lower-limb anatomy with options for:
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Partager
Participer à la discussion
Suggestions
Lundi 30 novembre -0001 de 00h à 00h (GMT+2)
Honolulu : Lundi 29 novembre 1999 de 12h à 12h (GMT-10)
San Francisco : Lundi 29 novembre 1999 de 14h à 14h (GMT-8)
New York : Lundi 29 novembre 1999 de 17h à 17h (GMT-5)
Buenos Aires : Lundi 29 novembre 1999 de 19h à 19h (GMT-3)
London / Dublin : Lundi 29 novembre 1999 de 22h à 22h (GMT)
Paris / Berlin : Lundi 29 novembre 1999 de 23h à 23h (GMT+1)
Istanbul : Mardi 30 novembre 1999 de 00h à 00h (GMT+2)
Moscou / Dubaï : Mardi 30 novembre 1999 de 02h à 02h (GMT+4)
Bangkok : Mardi 30 novembre 1999 de 05h à 05h (GMT+7)
Shanghai : Mardi 30 novembre 1999 de 06h à 06h (GMT+8)
Tokyo : Mardi 30 novembre 1999 de 07h à 07h (GMT+9)
Sydney : Mardi 30 novembre 1999 de 08h à 08h (GMT+10)
Wellington : Mardi 30 novembre 1999 de 10h à 10h (GMT+12)
San Francisco : Lundi 29 novembre 1999 de 14h à 14h (GMT-8)
New York : Lundi 29 novembre 1999 de 17h à 17h (GMT-5)
Buenos Aires : Lundi 29 novembre 1999 de 19h à 19h (GMT-3)
London / Dublin : Lundi 29 novembre 1999 de 22h à 22h (GMT)
Paris / Berlin : Lundi 29 novembre 1999 de 23h à 23h (GMT+1)
Istanbul : Mardi 30 novembre 1999 de 00h à 00h (GMT+2)
Moscou / Dubaï : Mardi 30 novembre 1999 de 02h à 02h (GMT+4)
Bangkok : Mardi 30 novembre 1999 de 05h à 05h (GMT+7)
Shanghai : Mardi 30 novembre 1999 de 06h à 06h (GMT+8)
Tokyo : Mardi 30 novembre 1999 de 07h à 07h (GMT+9)
Sydney : Mardi 30 novembre 1999 de 08h à 08h (GMT+10)
Wellington : Mardi 30 novembre 1999 de 10h à 10h (GMT+12)
Complex CTO: Ostial LAD CTO with ambiguous Proximal CAP
Case of the month: May 2019
Partager
Percutaneous EndoVascular Aortic Repair (PEVAR) with low profile endovascular graft
Case of the month: August 2017
Partager
Complex Acute Anterior STEMI with "no Reflow phenomenon" management
Case of the month: October 2018
Partager
TEVAR of the thoracic aneurysm with short neck below left common carotid artery using C TAG with act...
Case of the month: March 2022
Partager
Long Femoral Occlusion (35 cm) - Subintimal crossing and extra long stenting
Case of the month: July 2017
Partager
Complex Valve-in-Valve (VIV) TAVI for Aortic bioprosthesis dysfunction
Case of the month: July 2018
Partager











venkatesa reddy D. very good result
Mangesh T. My few questions about about Long Calcified SFA Recanalisation-
1.What was the prime aim of this Interventions to treat Proximal SFA Occlusion with Directional Atherectomy or Short segment occluded SFA?
2.Is Pre-dilatation with Coronary balloons (1.5-3.5mm) always necessary before Debulking of Femoro-Popliteal lesion with Atherectomy device?
3.Exact role of Chocolate Cutting balloon could not be understud? Why so many wires & balloons are used instead of doing Straightforward Hawkone Atherectomy and then Drug coated balloon plasty with In.pact Admiral?
4.Is their any loss of Paclitexel drug while doing Balloon Plasty multiple times?
5. After 'Inline flow' Recanalisation Why not below the knee Popliteo-tibial revascularisation Not attempted in same seating?
6.Does ABI Improved after long SFA Recanalisation & return of triphasic waveform in tibial arteries?
I feel Distal Embolisation protection device has No role in this Atherectomy + DEB Case!
So many hardware material uses is Luxury for IR Consultant!!
Do you agree with my comments?
Mangesh T. Great case done. Amazing results!!
Alexandre P. Interesting, than you